I never thought of myself as someone with food allergies. I indulge excessively in gluten, dairy, peanuts, and most other common allergens.
About five or six years ago, my mouth and throat started to itch a bit whenever I ate apples. I’m from Minnesota, home of the Honeycrisp, where apples are a main food group, and so I persevered through the irritation. Ignoring my symptoms was easier than dealing with the nuisance. What started with apples, however, grew to include avocados, cherries, almonds, and many other foods.

Photo by Shen Swartout
This past fall I had a constant rash around my mouth. I had been eating many apples, as they were in season, and wondered if cutting my apple consumption would help get rid of my rash. It subsided, but never vanished. In an effort to find out what was wrong with me, I began to research my symptoms.
Oral Allergy Syndrome (also known as pollen-food allergy syndrome) is the most common allergy you’ve never heard of. The American College of Allergy, Asthma, and Immunology explains that OAS is caused by “cross-reacting allergens found in both pollen and raw fruits, vegetables, or some tree nuts.” It goes on, explaining that cooking the foods deactivates the allergens and that the allergy doesn’t appear until late adolescence or early adulthood after someone has already eaten these foods for years.
Birch, grass, and ragweed pollen are to blame. Each infects different fruits, nuts, and vegetables. Seasonal allergies are often tied to OAS symptoms. I have experienced seasonal allergies for about as long as I have experienced OAS. Treatment is not usually necessary, as the allergy is very minor and more of an annoyance than anything.
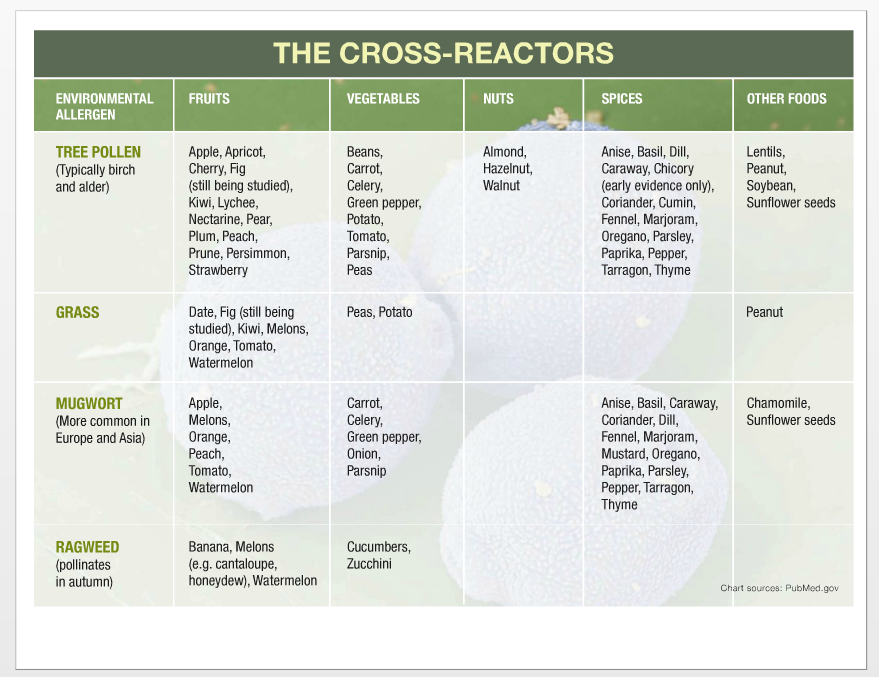
Photo courtesy of allergicliving.com
Some people, however, are at risk for anaphylaxis, or very severe reactions. I am one of them. Having OAS and getting a rash on your face after eating offending foods or symptoms when eating the foods cooked indicates a potential for anaphylaxis. The chances are slim – only about 1.7 percent of people with OAS – but the threat is real. Researching your own symptoms of OAS is worth it, but the information is not abundant.
For being the most common allergy in adults, you would expect to have heard of it. I’ve met many others with a similar reaction to certain produce. Yet, nobody I have talked to about OAS has ever heard of the affliction itself, though most know someone with this issue.

Photo by Shen Swartout
My experience with OAS has changed the way I eat. I no longer eat fruit with every meal, and my college dining hall is a horrible reminder of the foods I used to enjoy. Every time I hear the crunch of an apple, I think sadly about how I should probably never eat one again. I still risk it sometimes, indulging in guac with my friends or eating my favorite chocolate-covered almonds from Trader Joe’s.
I also try not to lose hope in the future. Science may someday advance to remedy food allergies in general, and preventing cross-pollination would prevent OAS symptoms. For those of you suffering with me, you are not alone.


